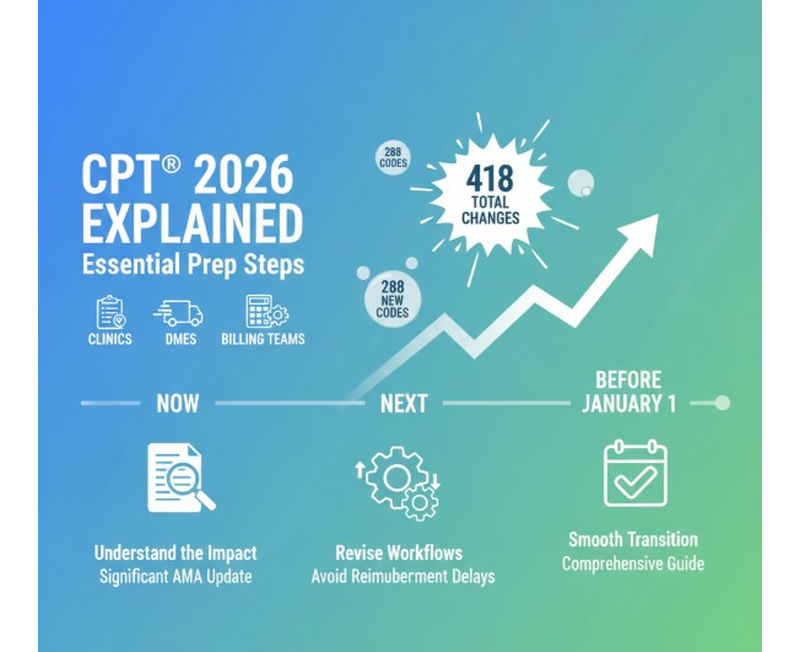
Every year, the healthcare industry braces for updates to the AMA’s CPT code set—but the 2026 update is one of the most significant in recent years. With 418 total changes, including 288 new CPT codes, medical practices, clinics, and DME providers need to begin preparing now to avoid reimbursement delays or operational disruptions.
Below is a comprehensive, practice-friendly guide to what’s changing, how it impacts your workflow, and what steps you can take to prepare before January 1, that can help you transition smoothly.
Summary of Key CPT 2026 Changes
The 2026 update brings sweeping adjustments across nearly every major section of CPT®. Here’s a snapshot of what’s new:
- 288 new CPT codes for medical, surgical, diagnostic, and emerging technologies
- 84 deletions of outdated or redundant codes
- 46 revisions impacting code descriptions, guidelines, or time durations
- All changes take effect Jan 1, 2026 (with payer adoption timelines varying)
Coders may feel relief this year, the Evaluation & Management (E/M) section remains largely unchanged, with only minor additions and revised guidance.
Clinics using CGM and remote monitoring services should pay close attention, as several new RPM and device-related codes (including CGM RPM billing) arrive with updated time thresholds.
Overall, practices must ensure that their documentation, coding workflows, and billing teams are aligned before the new year begins.
The Areas Affected Most in CPT 2026
Although many sections saw minor edits, others underwent major restructuring. Here are the most impactful areas for medical practices and DME suppliers:

✔ Surgery
This section saw one of the largest expansions:
- New lower extremity revascularization codes (37254–37299)
- Updated biopsy codes (55707–55715)
- New spinal decompression codes (62330–63032)
These changes affect procedural billing, prior authorizations, and clinical documentation.
✔ Radiology
A mix of deletions and new codes:
- Computed tomographic angiography reporting codes (70471–70473)
- New surface radiation therapy codes (77436–77439)
Imaging centers and oncology practices should prioritize training.
✔ Medicine Section
A high-volume area with notable additions:
- New RSV vaccine codes
- New hearing device evaluation and selection codes (92628, 92631)
- New codes for mechanical scalp cooling (97007–97009)
Primary care, ENT, audiology, oncology, and infusion centers will feel the biggest impact.
✔ Pathology & Laboratory
Ongoing additions and removals to proprietary laboratory analyses (PLA).
✔ Category III Codes
This section continues to grow rapidly, reflecting emerging technology:
- HIFU for benign prostate tissue
- Algorithmic burn-depth assessment
- Totally implantable middle-ear devices
- Selective enzymatic debridement
- Remote interrogation technology
These updates hint at the expanding role of AI, algorithms, and remote monitoring in clinical care.
What These Changes Mean for Your Medical Practice
CPT 2026 isn’t just a coding update—it’s an operational shift. These updates will directly impact how practices deliver care, document encounters, and get reimbursed.
✔ Reimbursement Risk
New codes mean:
- Increased risk of under-coding or over-coding
- Higher chance of denials if outdated codes are used
- Delayed payments if payers haven’t fully implemented changes
This is especially important in CGM billing and CGM RPM billing, where time-based codes are frequently audited.
✔ Documentation Requirements Will Tighten
New time requirements for RPM and CGM-related codes mean:
- More precise documentation
- Increased need for automated tracking
- Higher dependency on EHR accuracy
✔ Prior Authorizations Will See Shifts
Many new surgical and radiology codes will require updated authorization rules:
- Incorrect mapping could lead to denials
- Old CPT codes could get rejected if submitted after Jan 1
- Clinics need updated order sets and templates
✔ Coding Team Training Is No Longer Optional
With 418 changes, practices must invest in:
- Refresher coding sessions
- Compliance reviews
- Updated billing procedures
- Crosswalking old-to-new codes
A lack of preparation could significantly impact reimbursement for Q1 and Q2 of 2026.
Operational Adjustments Practices Should Make Now
To avoid revenue leakage, clinics and practices should implement these operational steps before the 2026 go-live date:

- Update Your EHR and PMS Systems
Ensure:
- New CPT codes are loaded
- Deleted codes are removed
- Documentation templates reflect new language
- Time-based RPM/CGM requirements are integrated
- Review Your Charge Master
Your internal fee schedule must align with:
- New CPT codes
- Revised code descriptions
- Updated payer-specific allowable amounts
- Train Your Coding, Billing & Clinical Teams
Training should include:
- Updated code sets
- New RPM/CGM RPM billing rules
- New vaccine and hearing evaluation codes
- Category III code usage
- Evaluate Your Prior Authorization Workflow
Specialties most affected:
- Orthopedics
- Cardiology
- Oncology
- Radiology
- Urology
Update checklists to ensure correct CPT codes are used.
- Communicate With Payers Early
Payer CPT adoption varies. Clinics should:
- Request updated fee schedules
- Confirm coverage for new Category III codes
- Validate timelines for CGM and RPM billing updates
- Run Internal Audits Before Jan 1
Conduct test claims to identify:
- Workflow gaps
- Mapping issues
- Potential denial trends
This proactive step can save months of correction later.
Conclusion
CPT 2026 is extensive, and the transition can feel overwhelming for practices that rely heavily on accurate coding and streamlined billing—especially when it comes to areas like CGM billing, CGM RPM billing, remote monitoring, and major specialty code updates. As payers adjust at different speeds and documentation rules tighten, practices need structured support to avoid compliance risks and prevent revenue disruptions. This is exactly where Med Karma steps in.
With over 27 years of industry expertise, Med Karma provides end-to-end support through every stage of the transition—from updating EHR, PMS, and billing systems with new CPT codes to helping teams understand specialty-specific changes that affect documentation and reimbursement. Our coding specialists assist practices in crosswalking old-to-new CPT codes, ensuring a seamless implementation without workflow confusion. We also conduct real-time claim audits to prevent early-year denials and offer continuous RCM oversight so your revenue remains stable during the transition period.
Beyond this, Med Karma supports sensitive, high-audit areas such as RPM, CGM, and surgical coding, and guides practices through the complexities of Category III technologies—covering documentation, payer requirements, and appeals. With our trained coders, auditors, and billing experts by your side, your practice can navigate CPT® 2026 confidently, accurately, and without interruption to cash flow. Med Karma ensures you’re fully prepared for the year ahead—operationally, clinically, and financially.