Med Karma Highlights How Accurate Verification Strengthens DME Billing Performance
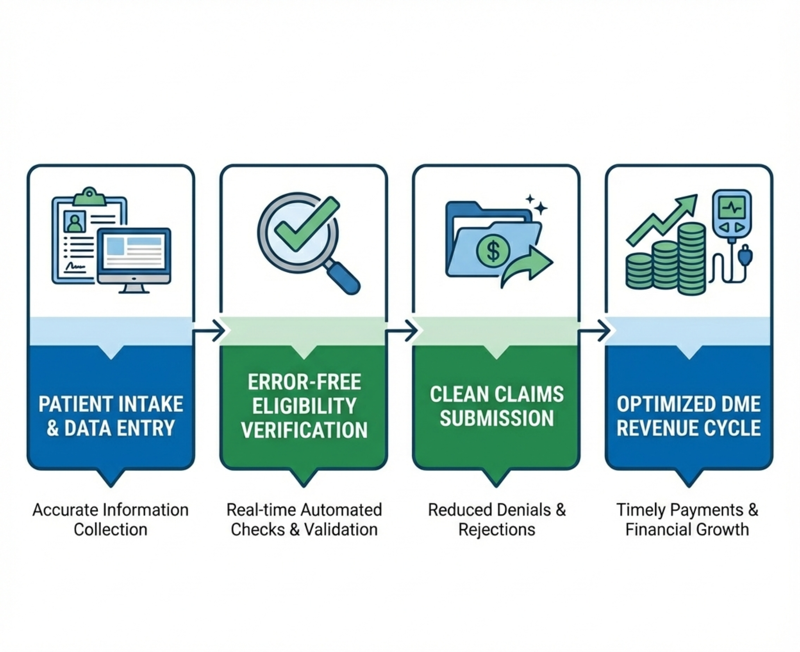
Durable Medical Equipment (DME) billing remains one of the most complex areas of healthcare revenue management. From shifting payer policies to strict compliance requirements, providers face persistent challenges that can result in denied claims, delayed reimbursements, and avoidable revenue loss.
Med Karma, a healthcare revenue cycle and billing support partner, emphasizes that one of the most effective ways to protect and grow revenue is by implementing accurate, reliable eligibility and benefits verification at the front end of the billing process.
Why Eligibility Verification Is Critical to DME Success
Eligibility and benefits verification confirm coverage, clarifies payer requirements, and establishes patient financial responsibility before equipment is dispensed. When verification is incomplete or inaccurate, providers risk claim denials, unreimbursed services, and patient dissatisfaction.
The Revenue Impact of Error-Free Verification
Strong verification practices support measurable improvements across the revenue cycle, including:
- Reduced claim denials and rejections through accurate insurance validation
- Improved cash flow driven by faster and cleaner claim submissions
- Greater operational efficiency by reducing rework and administrative burden
- Stronger patient trust through transparent financial communication
What to Look for in a Verification Partner
A reliable eligibility and benefits verification process should include comprehensive insurance validation, real-time policy updates, accurate documentation, and strict adherence to compliance standards such as HIPAA.
How Med Karma Supports DME Providers
Med Karma delivers structured, compliance-focused eligibility and benefits verification services designed to simplify billing workflows and maximize revenue outcomes. By reducing errors and streamlining processes, Med Karma helps providers focus more on patient care while maintaining stronger financial performance.
About Med Karma
Med Karma is a healthcare billing and revenue cycle management partner specializing in RCM, credentialing, patient contact solutions, and virtual assistance services. Med Karma supports healthcare organizations with scalable solutions that improve efficiency, compliance, and revenue outcomes.